Health
Understanding Pollen-Food Allergy Syndrome: Symptoms and Solutions

Pollen-Food Allergy Syndrome (PFAS) affects a significant portion of individuals who suffer from pollen allergies, with estimates suggesting that up to 70% experience this often overlooked condition. PFAS arises from cross-reactivity, where the body mistakenly identifies proteins in food as similar to those found in pollen. This confusion can lead to allergic reactions when consuming certain plant-based foods.
The typical response includes itching or swelling of the mouth, face, lips, tongue, and throat shortly after ingestion of foods such as fruits, vegetables, nuts, and legumes. Symptoms usually manifest as mild discomfort; however, more severe systemic reactions can occur in 2-10% of cases, underscoring the importance of accurate diagnosis and management.
Understanding the Mechanisms of PFAS
PFAS is rooted in complex immunological responses. It is estimated that over 60% of food allergies stem from cross-reactions between food and inhaled allergens. The range of affected individuals includes up to 20% of children and as many as 58% of adults. Different pollen types trigger different reactions; for instance, individuals allergic to birch pollen may react to peaches, apples, and hazelnuts, while those sensitive to grass or weed pollen might experience symptoms after consuming melons or bananas.
Geographical variability also plays a role, as specific pollen types are more prevalent in certain areas. The proteins responsible for PFAS, known as Class 2 allergens, are typically labile, meaning they can change structure when heated or digested. This characteristic explains why reactions are often limited to oral and gastrointestinal symptoms rather than respiratory ones.
Importance of Accurate Diagnosis
Diagnosing PFAS can prove challenging. A comprehensive patient history focused on symptoms, coupled with specific IgE blood testing, is crucial for identifying allergic triggers. When patients present with symptoms localized to the mouth and digestive tract after eating plant foods, it signals the need for a detailed allergy assessment.
In cases where seasonal respiratory symptoms coexist, clinicians often perform a thorough allergen sensitization profile tailored to the patient’s geographical context. This process not only confirms pollen and other environmental allergies but also informs personalized management plans. Such plans may include strategies for reducing exposure to allergens, such as avoiding certain foods during peak pollen seasons or altering food preparation methods, like peeling or cooking.
Accurate diagnosis not only distinguishes between PFAS and other food allergies but also helps in identifying the overall burden of allergens affecting the patient. With up to 80% of allergy sufferers being sensitive to multiple allergens, understanding the cumulative effects is vital for effective management.
In conclusion, recognizing and diagnosing Pollen-Food Allergy Syndrome is essential for improving patient outcomes. By shifting from reactive to proactive allergy management, healthcare providers can enhance quality of life for individuals grappling with this condition. Early intervention and tailored strategies can significantly reduce allergen exposure and alleviate symptoms, ultimately leading to a healthier lifestyle.
-

 Business1 week ago
Business1 week agoIconic Sand Dollar Social Club Listed for $3 Million in Folly Beach
-

 Politics1 week ago
Politics1 week agoAfghan Refugee Detained by ICE After Asylum Hearing in New York
-

 Health1 week ago
Health1 week agoPeptilogics Secures $78 Million to Combat Prosthetic Joint Infections
-

 Science1 week ago
Science1 week agoResearchers Achieve Fastest Genome Sequencing in Under Four Hours
-

 Health1 week ago
Health1 week agoResearcher Uncovers Zika Virus Pathway to Placenta Using Nanotubes
-

 Lifestyle1 week ago
Lifestyle1 week agoJump for Good: San Clemente Pier Fundraiser Allows Legal Leaps
-

 World1 week ago
World1 week agoUS Passport Ranks Drop Out of Top 10 for First Time Ever
-

 Entertainment1 week ago
Entertainment1 week agoJennifer Lopez Addresses A-Rod Split in Candid Interview
-

 Business1 week ago
Business1 week agoSan Jose High-Rise Faces Foreclosure Over $182.5 Million Loan
-
 Science1 week ago
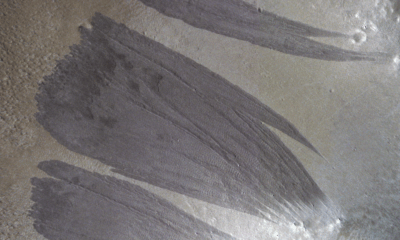
Science1 week agoMars Observed: Detailed Imaging Reveals Dust Avalanche Dynamics
-

 Top Stories6 days ago
Top Stories6 days agoChicago Symphony Orchestra Dazzles with Berlioz Under Mäkelä
-

 World1 week ago
World1 week agoRegional Pilots’ Salaries Surge to Six Figures in 2025