Health
Axi-Cel Expands Role in Treating Large B-Cell Lymphoma Patients

The use of axicabtagene ciloleucel (axi-cel; Yescarta) in treating patients with large B-cell lymphoma (LBCL) has significantly broadened, reflecting its demonstrated survival benefits over traditional chemotherapy. This advancement highlights the need to clarify the optimal role of CAR T-cell therapies within the evolving treatment landscape for this aggressive disease, according to Dr. Taylor Brooks, an associate staff physician at the Cleveland Clinic Taussig Cancer Institute in Ohio.
In a recent interview with OncLive®, Dr. Brooks emphasized the surge in research focused on cellular therapies for aggressive B-cell lymphomas. He noted that CAR T-cell therapies, specifically axi-cel, show superior efficacy compared to historical standard-of-care therapies for patients with relapsed or refractory LBCL. The implications of using axi-cel in second-line treatment settings pose challenges in determining subsequent treatment strategies for patients who experience disease relapse.
Research Findings on CAR T-Cell Therapy
The efficacy of CAR T-cell therapies, particularly axi-cel, has been underscored by data from various studies. A pivotal study, the ZUMA-1 trial, revealed that approximately 100 patients with refractory LBCL treated with axi-cel achieved an overall response rate of 82%, with a complete response rate of 54%. Long-term follow-up indicated that 31% of these patients maintained a complete response lasting an average of five years.
Building on the success of later-line therapies, the ZUMA-7 trial aimed to evaluate the efficacy of axi-cel as a first-line treatment for patients with primary refractory disease. In this head-to-head trial, patients who did not achieve a complete response to frontline therapy or relapsed within twelve months were randomly assigned to receive either axi-cel or salvage chemotherapy. The results were striking: 65% of the axi-cel group achieved a complete response compared to only 32% in the standard-of-care group. Moreover, the 24-month event-free survival rate was 41% for axi-cel patients versus just 16% for those receiving standard therapy.
The median overall survival for patients in the axi-cel group was not reached, whereas it was only 31.1 months for those treated with chemotherapy and transplant. Even after adjusting for subsequent off-protocol cellular immunotherapy received by many in the standard care group, analyses continued to support improved overall survival with axi-cel.
In April 2022, the Food and Drug Administration (FDA) approved axi-cel for treating patients with primary refractory or early relapsed LBCL, marking a significant milestone in the management of this condition.
Future Directions in Treatment Strategies
While the approval of axi-cel enhances treatment options, it raises questions about the best subsequent therapies for patients who relapse after initial treatment. The emergence of bispecific antibodies represents a new class of medications that may play a vital role in addressing this challenge. Although they exhibit modest single-agent activity, these therapies are increasingly being explored in combination with various agents, including targeted therapies and conventional chemotherapy.
One of the most anticipated studies is the ZUMA-23 trial (NCT05605899), which is currently enrolling patients with high-risk LBCL. This phase 3 trial investigates the application of CAR T-cell therapies in the first-line setting for patients with poor prognostic factors. The findings are expected to significantly influence treatment paradigms, potentially establishing CAR T-cell therapy as a standard option even for treatment-naïve patients.
The advancements in CAR T-cell therapies, particularly the results from ongoing studies like ZUMA-23, could revolutionize the therapeutic landscape for LBCL, promising better outcomes for patients facing this challenging disease. As research continues to unfold, the integration of innovative treatments will be crucial in improving survival rates and overall patient care in the field of hematologic malignancies.
-

 Science1 month ago
Science1 month agoUniversity of Hawaiʻi Leads $25M AI Project to Monitor Natural Disasters
-
 Science2 months ago
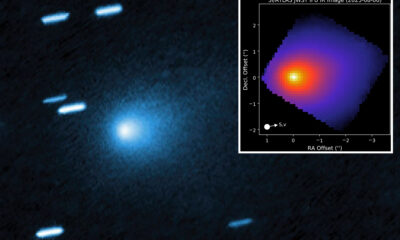
Science2 months agoInterstellar Object 3I/ATLAS Emits Unique Metal Alloy, Says Scientist
-

 Science2 months ago
Science2 months agoResearchers Achieve Fastest Genome Sequencing in Under Four Hours
-

 Business2 months ago
Business2 months agoIconic Sand Dollar Social Club Listed for $3 Million in Folly Beach
-

 Politics2 months ago
Politics2 months agoAfghan Refugee Detained by ICE After Asylum Hearing in New York
-

 Business2 months ago
Business2 months agoMcEwen Inc. Secures Tartan Lake Gold Mine Through Acquisition
-

 Health2 months ago
Health2 months agoPeptilogics Secures $78 Million to Combat Prosthetic Joint Infections
-
 Science2 months ago
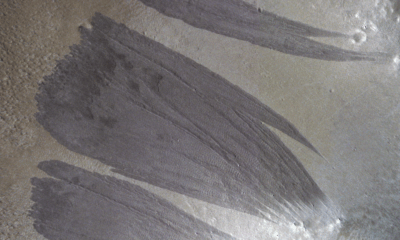
Science2 months agoMars Observed: Detailed Imaging Reveals Dust Avalanche Dynamics
-

 Lifestyle2 months ago
Lifestyle2 months agoJump for Good: San Clemente Pier Fundraiser Allows Legal Leaps
-

 Health2 months ago
Health2 months agoResearcher Uncovers Zika Virus Pathway to Placenta Using Nanotubes
-

 Entertainment2 months ago
Entertainment2 months agoJennifer Lopez Addresses A-Rod Split in Candid Interview
-

 World2 months ago
World2 months agoUS Passport Ranks Drop Out of Top 10 for First Time Ever