Health
Optum Launches Real-Time Claims Management System at HLTH Conference

Optum, the data analytics division of UnitedHealth Group, unveiled its new claims management system, Optum Real, at the annual HLTH conference held in Las Vegas. This innovative platform aims to streamline the claims submission and reimbursement process, addressing growing concerns from healthcare providers about delays and denials often associated with insurance claims.
The introduction of Optum Real comes at a critical time, as frustration among providers has escalated over perceived insurer practices of “delay and deny.” During the conference, executives from Optum explained that while most claims are processed efficiently, a minority can cause significant headaches due to a lack of transparency in the system. Puneet Maheshwari, senior vice president and general manager of Optum Real, emphasized the importance of eliminating guesswork in claims and reimbursement, stating, “If I have to summarize it in one word, I would say the biggest challenge in claims and reimbursement is guesswork.”
Optum Real is described as a “multi-payer platform” that facilitates real-time data exchange between healthcare providers and payers, enabling the immediate identification of issues during claim submission. The system aims to reduce the administrative burden on both parties, which often leads to unnecessary costs. According to a press release from Optum, UnitedHealthcare, a subsidiary of the same parent company, is the first health plan to implement this technology.
Transforming Claims Processing
In a post-panel interview, Maheshwari elaborated on the current state of claims processing, which can take weeks or even months. He noted that the traditional method involves multiple stages where claims are sent in batches, leading to delays and potential errors. “The reason for that current state is because there’s a lack of transparency between payers and providers,” he said. “What real-time transparency enables is that it removes the guesswork.”
The goal of Optum Real is to provide immediate clarity during patient encounters. For instance, when a patient arrives for an MRI, the provider can quickly verify coverage and understand any associated costs before the service is rendered. Maheshwari highlighted that real-time queries allow for decisions to be made on the spot, significantly reducing the time from service delivery to payment.
This new approach also addresses the variability in healthcare services, where different procedures can lead to different coding and billing challenges. By integrating ambient scribing technology, Optum Real aims to ensure that documentation is accurate and complete in real time, facilitating a smoother claims process.
Challenging Industry Norms
Some skepticism remains regarding the feasibility of achieving true real-time processing in healthcare, a sector known for its slower pace. Maheshwari acknowledged this concern but asserted that Optum Real is designed to bridge the gap between providers and payers, fostering an environment of collaboration rather than competition. “The way to solve it is to create that real-time transparency,” he explained.
The financial implications of this system are significant. The healthcare industry currently experiences an estimated $300 billion to $350 billion in administrative costs related to claims processing. By enhancing transparency and efficiency, Optum Real aims to reduce these unnecessary expenses while improving the overall reimbursement experience for providers.
Despite the promising outlook, questions linger about how this initiative will reshape traditional insurance business models, which are often built on minimizing payouts. Maheshwari noted that while historical practices may present challenges, the majority of claims—approximately 80%—are successfully approved and paid without issue. The remaining claims that require reworking often stem from insufficient information during the initial submission.
As Optum Real begins implementation, health systems like Allina Health in Minnesota have already reported savings attributed to the new system. The broader impact on providers across the country will become clearer as more organizations adopt this technology.
In conclusion, the launch of Optum Real represents a significant step toward resolving long-standing issues in claims management. As providers and payers begin to navigate this new landscape, the healthcare community will closely monitor the effectiveness of this innovative solution in enhancing transparency and efficiency in the claims process.
-

 Business1 week ago
Business1 week agoIconic Sand Dollar Social Club Listed for $3 Million in Folly Beach
-

 Politics1 week ago
Politics1 week agoAfghan Refugee Detained by ICE After Asylum Hearing in New York
-

 Health1 week ago
Health1 week agoPeptilogics Secures $78 Million to Combat Prosthetic Joint Infections
-

 Science1 week ago
Science1 week agoResearchers Achieve Fastest Genome Sequencing in Under Four Hours
-

 Lifestyle1 week ago
Lifestyle1 week agoJump for Good: San Clemente Pier Fundraiser Allows Legal Leaps
-

 Health1 week ago
Health1 week agoResearcher Uncovers Zika Virus Pathway to Placenta Using Nanotubes
-

 World1 week ago
World1 week agoUS Passport Ranks Drop Out of Top 10 for First Time Ever
-

 Entertainment1 week ago
Entertainment1 week agoJennifer Lopez Addresses A-Rod Split in Candid Interview
-

 World1 week ago
World1 week agoRegional Pilots’ Salaries Surge to Six Figures in 2025
-
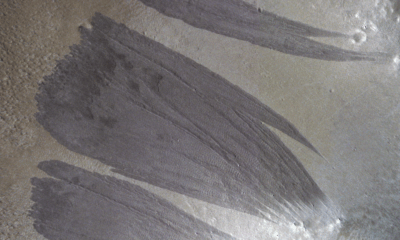
 Science1 week ago
Science1 week agoMars Observed: Detailed Imaging Reveals Dust Avalanche Dynamics
-

 Top Stories6 days ago
Top Stories6 days agoChicago Symphony Orchestra Dazzles with Berlioz Under Mäkelä
-

 Business1 week ago
Business1 week agoMcEwen Inc. Secures Tartan Lake Gold Mine Through Acquisition