Science
New Biomarkers Transform Non-Small Cell Lung Cancer Management

The management of non-small cell lung cancer (NSCLC) is entering a new phase as advancements in biomarker testing evolve beyond traditional genomic analysis. This shift, highlighted by Dr. Soo-Ryum (Stewart) Yang at the 20th Annual New York Lung Cancers Symposium on November 15, 2025, incorporates a range of protein-based and computational markers. These developments are largely inspired by the approval of innovative therapies, particularly antibody-drug conjugates (ADCs), and a better understanding of therapeutic resistance.
Dr. Yang, an assistant attending pathologist and co-director of Clinical Biomarker Development at Memorial Sloan Kettering Cancer Center, identified four pivotal trends in his presentation. The first trend is the increased use of protein-based immunohistochemistry (IHC) biomarkers to guide ADC therapies. He emphasized the importance of tumor suppressor genes, the potential of synthetic lethality in treatment approaches, and the growing role of computational pathology in informing clinical decisions.
Despite these advancements, a significant challenge persists: the scarcity of tissue samples. To tackle this issue, Dr. Yang advocated for the development of multiplex IHC methods and the integration of broad panel next-generation sequencing (NGS) alongside artificial intelligence. This approach aims to extend personalized therapies to a larger segment of the NSCLC patient population.
As part of this evolving landscape, the focus is shifting from solely identifying mutated genes to measuring the expression levels of specific proteins on cancer cells. This shift opens new avenues for treatment, particularly with established biomarkers such as PD-L1 used for checkpoint inhibitor therapy, now being applied to ADCs as well. Dr. Yang pointed out two critical protein biomarkers in NSCLC: HER2 and c-MET overexpression.
HER2 overexpression can be found in up to 20% of NSCLC patients, with the highest levels (IHC 3+) occurring in about 3%. Dr. Yang clarified that there is no direct correlation between HER2 mutation status and its overexpression. While the majority of NSCLC cases exhibiting high-level gene amplification will show IHC 3+ staining, not all 3+ cases are attributed to gene amplification.
The FDA’s approval of fam-trastuzumab deruxtecan-nxki (T-DXd; Enhertu) for HER2-positive solid tumors, including NSCLC patients who have undergone prior treatments, was bolstered by the phase 2 DESTINY-Lung01 study (NCT03505710) that applied HER2 scoring guidelines from gastric cancer. Dr. Yang proposed that these guidelines should now be adapted for NSCLC testing.
In the case of c-MET overexpression, Dr. Yang reported that this biomarker is common in NSCLC, with an actionable c-MET high status—defined as over 50% of tumor cells exhibiting 3+ staining—identified in up to 17% of EGFR wild-type cases. The FDA granted accelerated approval to telisotuzumab vedotin-tllv (teliso-V; Emrelis) for this patient group, supported by data from the phase 2 LUMINOSITY trial (NCT03539536).
Dr. Yang highlighted the need for a flexible diagnostic approach to integrate HER2 and c-MET IHC screening into current workflows, as there is no one-size-fits-all solution. He suggested that institutions should develop optimized workflows based on multidisciplinary input and available resources.
Several promising biomarkers under investigation could refine personalized treatment further. KRAS mutations, which occur in up to 40% of lung adenocarcinomas, are particularly noteworthy. The most common mutation, KRAS G12C, is followed by G12V and G12D mutations. The latter are associated with a history of light or non-smoking, a lower tumor mutational burden, and poorer response rates to chemoimmunotherapy.
Established therapies targeting KRAS G12C, including sotorasib (Lumakras) and adagrasib (Krazati), are already in use. Emerging therapies targeting other KRAS mutations are also being explored in clinical trials. For instance, Dr. Yang mentioned zoldonrasib (RMC-9805), a KRAS G12D inhibitor that demonstrated an overall response rate of 61% in a phase 1 study (NCT06040541).
Additionally, STK11 and KEAP1 mutations, which occur in up to 20% of lung cancers, often co-occur with KRAS mutations and contribute to an immunosuppressive tumor microenvironment. These mutations are linked to resistance to immunotherapy and are considered biomarkers of poor response to PD-1/PD-L1 inhibitors.
Data from the phase 3 POSEIDON trial (NCT03164616) suggests strategies to overcome this resistance. Adding a CTLA-4 inhibitor to PD-L1 therapy and chemotherapy improved progression-free survival (PFS) and overall survival (OS) for these patients, positioning STK11/KEAP1 mutations as potential indicators for more aggressive immunotherapy approaches.
Dr. Yang discussed the role of MTAP deletions, present in up to 18% of lung cancers, which create a metabolic vulnerability that can be exploited through synthetic lethality. Detection methods for MTAP include NGS, which can identify homozygous deletions without requiring additional tissue, and IHC, which can detect loss of MTAP protein expression.
Despite the advancements, Dr. Yang emphasized that tissue availability remains a critical issue. He noted the increasing demand for testing an expanding list of biomarkers from the same small biopsy samples.
Another key player in NSCLC treatment is the cell surface protein TROP2, which has garnered attention for ADC development. The anti-TROP2 ADC, datopotamab deruxtecan-dlnk (Dato-DXd; Datroway), is being investigated as a second-line treatment. Results from the phase 3 TROPION-Lung01 study (NCT04656652) indicated a PFS benefit with Dato-DXd compared to docetaxel, although no significant OS benefit was observed.
To enhance predictive power, Dr. Yang described an AI-driven method developed to analyze TROP2 expression using computational pathology. This technique scans IHC slides, allowing for a quantitative assessment of TROP2 staining, which could predict higher response rates and longer PFS with Dato-DXd. Although promising, he noted that this method requires further validation in prospective studies.
The advancements in NSCLC management represent a significant shift towards a comprehensive approach that integrates protein analysis, AI-driven techniques, and innovative therapies. As Dr. Yang stated, “We’re at a point where we should be starting to explore the feasibility of multiplex IHC similar to what we did with molecular markers and NGS.” The future of NSCLC treatment lies in the comprehensive use of broad-panel NGS and IHC, enhanced by AI, to refine biomarker testing and improve patient outcomes.
-
 Science4 weeks ago
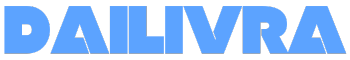
Science4 weeks agoInterstellar Object 3I/ATLAS Emits Unique Metal Alloy, Says Scientist
-

 Science4 weeks ago
Science4 weeks agoResearchers Achieve Fastest Genome Sequencing in Under Four Hours
-

 Politics1 month ago
Politics1 month agoAfghan Refugee Detained by ICE After Asylum Hearing in New York
-

 Business4 weeks ago
Business4 weeks agoIconic Sand Dollar Social Club Listed for $3 Million in Folly Beach
-

 Health1 month ago
Health1 month agoPeptilogics Secures $78 Million to Combat Prosthetic Joint Infections
-

 Business1 month ago
Business1 month agoMcEwen Inc. Secures Tartan Lake Gold Mine Through Acquisition
-

 Lifestyle1 month ago
Lifestyle1 month agoJump for Good: San Clemente Pier Fundraiser Allows Legal Leaps
-
 Science1 month ago
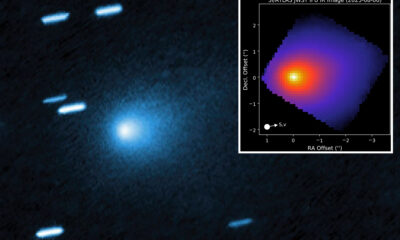
Science1 month agoMars Observed: Detailed Imaging Reveals Dust Avalanche Dynamics
-

 Health4 weeks ago
Health4 weeks agoResearcher Uncovers Zika Virus Pathway to Placenta Using Nanotubes
-

 World1 month ago
World1 month agoUS Passport Ranks Drop Out of Top 10 for First Time Ever
-

 Entertainment1 month ago
Entertainment1 month agoJennifer Lopez Addresses A-Rod Split in Candid Interview
-

 Business1 month ago
Business1 month agoSan Jose High-Rise Faces Foreclosure Over $182.5 Million Loan