Health
ctDNA Status Outperforms PET-CT in Predicting Lymphoma Outcomes
New findings presented at the 2025 ASH Annual Meeting and Exposition indicate that circulating tumor DNA (ctDNA) status at the end of treatment (EOT) serves as a more precise predictor of event-free survival (EFS) in lymphoma patients than traditional imaging methods like PET-CT. This retrospective analysis included real-world data from 144 patients across various lymphoma subtypes, demonstrating that ctDNA can significantly enhance prognostic capabilities in clinical settings.
The study revealed that patients with a ctDNA minimal residual disease (MRD)–negative status at EOT did not reach a median EFS, while those with ctDNA-MRD-positive status had a median EFS of just 1.97 months. Statistical analysis showed an adjusted hazard ratio (HR) of 22.43 (95% CI, 6.76-74.45; P < .0001), highlighting the stark difference in outcomes based on ctDNA status. In contrast, the 12- and 24-month HRs for the ctDNA-MRD-negative group were 0.83 and 0.79, respectively, indicating a more favorable prognosis.
The lead author, Dr. Natalie Galanina, a clinician investigator at UPMC Hillman Cancer Center in Pittsburgh, Pennsylvania, emphasized the importance of ctDNA assessment. “EOT ctDNA status can clarify ambiguous imaging results and enables earlier relapse detection,” she stated during the presentation. The study aims to bridge gaps in understanding ctDNA’s prognostic capabilities across diverse lymphoma types, particularly beyond diffuse large B-cell lymphoma (DLBCL).
To conduct the study, researchers prospectively collected 1,105 plasma samples from the patient cohort, which included a range of aggressive and indolent lymphomas. Most patients were male, with a median age of 61 years, and a majority presented with advanced stage IV disease. The median follow-up period for both EFS and overall survival (OS) was 20 months and 21 months, respectively.
The analysis showed that ctDNA presence was detectable in 94% of patients prior to treatment. The median number of tumor molecules per milliliter was approximately 100 for aggressive lymphomas and around 20 for indolent types, reflecting variations in circulating tumor burden.
In comparing ctDNA with traditional imaging, the results were striking. Patients with a negative PET-CT at EOT had a median EFS that was not achieved, while those with a positive PET-CT had a median EFS of 5.16 months (adjusted HR, 8.68; P = .0010). Conversely, negative ctDNA-MRD at EOT indicated a median EFS that was not achieved, compared to 2.04 months for positive ctDNA-MRD (adjusted HR, 49.77; P < .0001). Dr. Galanina noted that integrating ctDNA as an adjunct to EOT assessment could help further stratify patients at risk of relapse. “For patients who are EOD PET-negative but ctDNA positive, this may inform post-treatment surveillance,” she explained. “In contrast, PET-positive patients who are MRD-negative may not require additional therapy, as 75% of them do not progress.”
The study also highlighted the prognostic significance of ctDNA clearance during frontline therapy. Patients who cleared their ctDNA had a median EFS that was not achieved, while those who did not clear ctDNA had a median EFS of 2.05 months (adjusted HR, 8.57; P = .0005). This suggests that early clearance could inform potential de-escalation of therapy, particularly for older patients or those with comorbidities.
Moreover, the findings indicated that ctDNA clearance maintained its predictive value in patients undergoing CAR T-cell therapy. Most MRD-positive patients who cleared ctDNA within three months post-CAR T achieved durable remission after one year.
In conclusion, Dr. Galanina emphasized the need for integrating ctDNA testing into routine clinical management for lymphoma care. “MRD assessment supports the use of ctDNA testing to personalize treatment and improve outcomes for patients,” she stated, underscoring the potential for enhanced patient monitoring and tailored therapies.
Overall, this analysis reinforces the superiority of ctDNA status as a prognostic tool, offering new avenues for improving clinical outcomes in lymphoma treatment.
-

 Science1 month ago
Science1 month agoUniversity of Hawaiʻi Leads $25M AI Project to Monitor Natural Disasters
-
 Science2 months ago
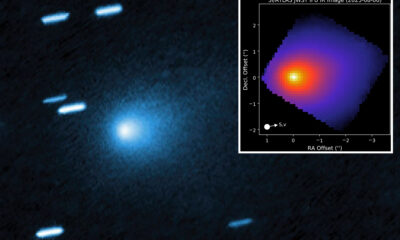
Science2 months agoInterstellar Object 3I/ATLAS Emits Unique Metal Alloy, Says Scientist
-

 Science2 months ago
Science2 months agoResearchers Achieve Fastest Genome Sequencing in Under Four Hours
-

 Lifestyle1 week ago
Lifestyle1 week agoSend Holiday Parcels for £1.99 with New Comparison Service
-

 Business2 months ago
Business2 months agoIconic Sand Dollar Social Club Listed for $3 Million in Folly Beach
-

 Politics2 months ago
Politics2 months agoAfghan Refugee Detained by ICE After Asylum Hearing in New York
-

 Business2 months ago
Business2 months agoMcEwen Inc. Secures Tartan Lake Gold Mine Through Acquisition
-

 Health2 months ago
Health2 months agoPeptilogics Secures $78 Million to Combat Prosthetic Joint Infections
-
 Science2 months ago
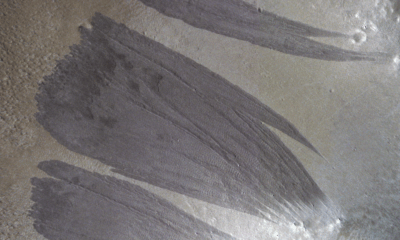
Science2 months agoMars Observed: Detailed Imaging Reveals Dust Avalanche Dynamics
-

 Lifestyle2 months ago
Lifestyle2 months agoJump for Good: San Clemente Pier Fundraiser Allows Legal Leaps
-

 Health2 months ago
Health2 months agoResearcher Uncovers Zika Virus Pathway to Placenta Using Nanotubes
-

 Entertainment2 months ago
Entertainment2 months agoJennifer Lopez Addresses A-Rod Split in Candid Interview