Health
Navigating Migraine Management After Surgery: A Personal Journey

After enduring a major surgery for an external tibia/fibula break and a complex tibial plateau break, a patient faced the added challenge of a debilitating migraine that lasted 19 days. Following her experience, she highlights the importance of advocating for appropriate migraine treatment in hospital settings.
Challenging Recovery Journey
The ordeal began on December 17, 2024, when the patient, after a hike with her puppy, suffered a fall that resulted in serious injuries. Rushed to the hospital, she underwent her first major surgery and was prescribed a strict regimen of care, which included being non-weight bearing for 12 weeks and a lengthy recovery period. Complications arose when the bones did not heal as expected, necessitating a second surgery to replace surgical hardware.
Just days after this second procedure, while transferring to a rehabilitation center, she experienced the onset of a migraine. According to research, such postoperative migraine headaches can be linked to general anesthesia and opioid use. Unfortunately, her new medical team was not familiar with her migraine medications, which added to her distress.
Initially, the rehabilitation staff placed her in charge of her own migraine medications. As her condition worsened, she realized the risk of “rebound” headaches and sought assistance from her headache specialist. The response from her floor doctor was disheartening; he expressed concerns that starting a Medrol dose pack could impede her healing process. This left her in a difficult position: endure the migraine indefinitely or risk further complications in her recovery.
Advocating for Better Care
During her rehabilitation, the patient observed a significant knowledge gap among healthcare providers regarding migraine treatment. Many staff members viewed her condition as merely a “bad headache,” unaware of the severity of her situation. The lack of training in headache medicine is a well-documented issue; a study highlighted that many medical schools do not include proper headache training in their curricula, leaving primary care physicians ill-equipped to treat these conditions effectively.
After a grueling 16 days, she successfully contacted her headache specialist, who arranged for her to receive IV infusions at her office. The relief was palpable; the expert administered necessary treatments, including nerve blocks, which ultimately alleviated her migraine. Following this intervention, she made significant strides in her physical and occupational therapy.
While she remains cautious about the potential return of her migraine, this experience served as a wake-up call. The patient not only managed her own health crisis but also educated some staff about migraines—what they entail and the various treatment options available. Yet, she reflects on the broader challenge that persists in healthcare: the need for greater awareness and understanding of migraine management.
As this patient navigated her recovery, she encountered a complex healthcare landscape that often overlooks the intricacies of migraine treatment. Her story underscores the critical need for improved education and resources for medical professionals, ensuring that patients receive the comprehensive care they deserve.
-
 Science3 weeks ago
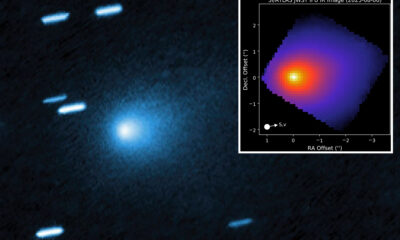
Science3 weeks agoInterstellar Object 3I/ATLAS Emits Unique Metal Alloy, Says Scientist
-

 Politics3 weeks ago
Politics3 weeks agoAfghan Refugee Detained by ICE After Asylum Hearing in New York
-

 Science3 weeks ago
Science3 weeks agoResearchers Achieve Fastest Genome Sequencing in Under Four Hours
-

 Business3 weeks ago
Business3 weeks agoIconic Sand Dollar Social Club Listed for $3 Million in Folly Beach
-

 Health3 weeks ago
Health3 weeks agoPeptilogics Secures $78 Million to Combat Prosthetic Joint Infections
-

 Lifestyle3 weeks ago
Lifestyle3 weeks agoJump for Good: San Clemente Pier Fundraiser Allows Legal Leaps
-
 Science3 weeks ago
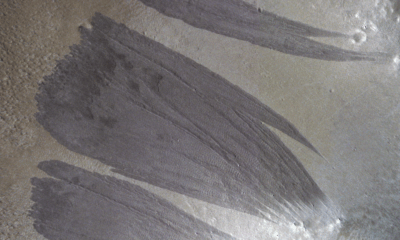
Science3 weeks agoMars Observed: Detailed Imaging Reveals Dust Avalanche Dynamics
-

 World3 weeks ago
World3 weeks agoUS Passport Ranks Drop Out of Top 10 for First Time Ever
-

 Health3 weeks ago
Health3 weeks agoResearcher Uncovers Zika Virus Pathway to Placenta Using Nanotubes
-

 Entertainment3 weeks ago
Entertainment3 weeks agoJennifer Lopez Addresses A-Rod Split in Candid Interview
-

 Business3 weeks ago
Business3 weeks agoSan Jose High-Rise Faces Foreclosure Over $182.5 Million Loan
-

 Top Stories3 weeks ago
Top Stories3 weeks agoChicago Symphony Orchestra Dazzles with Berlioz Under Mäkelä